Peptic Ulcer Disease (PUD)
What are Peptic Ulcers ?
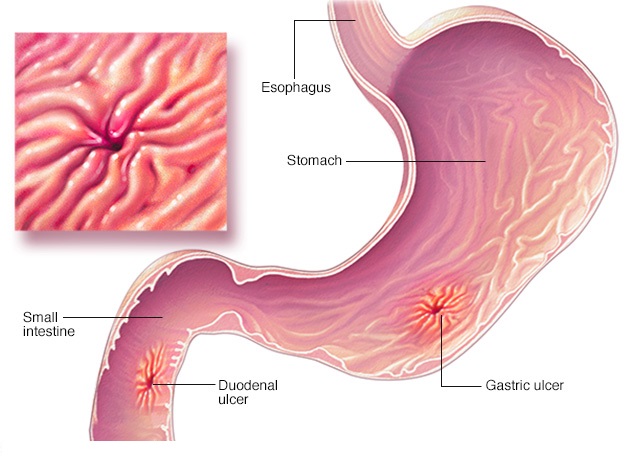
Peptic ulcer disease (PUD), otherwise known as a stomach ulcer or gastric ulcer, is a collective term used to describe aberrations (variations from the normal condition) in the gastrointestinal tract lining, including the stomach and portions of the stomach’s small intestine.
This condition is often associated with delicate or significant breaks in the stomach’s inner lining in the case of stomach or gastric ulcers, the duodenum in duodenal ulcers or even the lower portions of the oesophagus in rare cases. To better understand the delicate nuances between the main forms of this condition, we must first take a look at a couple of definitions used throughout:
- An ulcer refers to an open sore in the internal or external lining of body tissues that fail to heal, particularly the mucous membrane. These may range from simple sores to large lesions (major tissue damage).
- The Stomach is a bag of muscle tasked with digesting food located in the upper abdomen. However, it is more commonly used to refer to the general region of the lower abdomen when describing pains or feelings of distress (often known as the ‘belly aches’ or ‘tummy aches’). It is connected to the oesophagus above it and the small intestine below it. Gastric ulcers refer to ulcers within the stomach lining.
- The small intestine (or small bowel) is midway in the gastrointestinal tract connecting the stomach to the large intestine tasked with the absorption of various nutrients. It comprises of three major, consecutive regions – the duodenum, ileum and jejunum in that order – of which only the duodenum is of interest when characterising peptic ulcers. Duodenal ulcers refer to ulcers within the duodenum of the small intestine.
What are the common symptoms of Peptic Ulcer Disease ?
The leading symptom of this disease is characterised by a sensation of ‘burning pains’ or ‘dull aches’ in the general abdominal region. It is also sometimes described as a feeling of rolling discomfort (or ‘gas’) and accompanied by dry belching (or ‘burps’)
What is the differentiating Between a Gastric Ulcer and Duodenal Ulcer ?
An individual may suffer separately from ulcers of the stomach and duodenum or even from a combination of both (referred to as gastroduodenal ulcers). The key difference between the two lies in the onset and location of symptoms and not from the symptoms themselves. For instance, the onset of pain (i.e. a symptom) may be in the time between meals (in the case of duodenal ulcers) or triggered due to the meals themselves (in the case of gastric ulcers), which can help better diagnose the exact form of ulcer. However, in some cases, the pain may be referred (away from the actual area in which it is localised), such as duodenal ulcers being referred to the upper right quadrant of the abdomen.
What are the causes of Stomach Ulcer ?
Peptic ulcers can result from a few different types of issues; most of them are commonly linked to either an infection or drug side-effect. Some of the common causes have been elaborated below:
- Helicobacter pylori is an infectious bacterium that is most commonly associated with peptic ulcers. Typically, pathogens are killed in a highly acidic environment. However, this bacterium creates an alkaline environment within the stomach by secreting urease, thus enabling it to survive and cause inflammation and infection in the
- NSAIDs such as aspirin can increase the risk of a peptic ulcer up to four times. Additionally, other medications that can react with NSAIDs such as SSRIs, corticosteroids, anti-mineral corticosteroids and anticoagulants can further increase the risk.
- Stress has also been reported as an evident cause of peptic ulcers. Such forms are conveniently known as stress ulcers.
- A specific type of diet may predispose an individual to peptic ulcers, such as those rich in spice, coffee and
- Underlying conditions of gastric ischaemia (lack of blood supply to organs in the GI tract), vasculitis (inflammatory destruction of blood vessels) or Crohn’s disease (IBD) can also contribute to an increased risk of peptic ulcers.
Fact: The internal environment of the stomach has a pH between 1.5 to 3.5. To put that into perspective, it is just a few points below the pH of lead battery acid!
What are the symptoms of a Peptic Ulcer ?
Most of the symptoms experienced by a patient are from internal bleeding. But in severe cases, there are a few obvious symptoms that can be of diagnostic relevance, such as:
- Epigastric pain and burning sensations (pain in the upper central region of the abdomen).
- Bloating or feelings of abdominal fullness.
- Waterbrash, sometimes called ‘acid reflux’, refers to dilute acid’s regurgitation into the
- Nausea and persistent
- Loss of appetite and subsequent loss of weight (in case of gastric ulcers).
- Gain n weight (in case of duodenal ulcers).
- Hematemesis (vomiting of blood) due directly to gastric ulcers or due to damage to the oesophagus due to repeated regurgitation.
- Melena (foul-smelling or and tarry faeces).
- Acute peritonitis (inflammation of the inner wall lining the abdomen) in very severe cases, leading to extreme ‘stabbing’ pain.
- Heartburn (burning sensation in the upper chest) or gastroesophageal reflux disease (GERD).
- Certain medications that cross-react with non-steroid anti-inflammatory drugs (NSAIDs) such as steroids, anticoagulants, selective serotonin reuptake inhibitors (SSRIs), alendronate, risedronate
Fact: Nearly 75 per cent of patients who suffer from gastric or duodenal ulcers do not show or report any apparent symptoms
What are the treatment options ?
Stomach Ulcer Treatment
The type of treatment strategy to be administered depends entirely on the cause or origin of the peptic ulcer. The major courses of action depending on the root cause of the ulcer include:
- Antibiotics to kill pylori (e.g. amoxicillin, tetracycline, levofloxacin, metronidazole etc.)
- Antacids such as proton-pump inhibitors and, at times, bismuth subsalicylate.
- Acid blockers or histamine blockers to reduce stomach acid production and relieve.
- Cytoprotective agents to help seal and protect the inner lining of the stomach and small.
Managing Ulcer Pain
The foremost management strategy for pain is eradication therapy. Once H. pylori have been confirmed, treatment using antibiotics such as pantoprazole, clarithromycin, amoxicillin and metronidazole can help remove the infection and the ulcer pain.
Alternatively, treatment by removing NSAIDs from the prognosis can help mitigate medication-associated ulcers.
Remember
Overall, the condition is rarely fatal unless it presents with a horde of other complications such as internal bleeding or perforations. More often than not, it can be prevented by maintaining a healthy diet or by addressing any abdominal distress promptly instead of waiting for it to subside.
What is the best antacid for a stomach ulcer?
There is no one particular best antacid since it depends on the severity of symptoms and is usually prescribed at the merit of a physician.
Do peptic ulcers spread?
Ulcers caused due to H. pylori infections will spread through faeces.
The pain due to ulcers can feel like burning, stabbing or gnawing sensations in the stomach or lower abdominal region.
What does a peptic ulcer feel like?
Do peptic ulcers go away?
In minor cases, yes. But it is always advisable to consult a physician to be certain.


